A 65 year-old man with CAD s/p PCI c/b ICM/HFrEF (LVEF 38%) initially presents with an acute onset of aphasia, dysarthria, and right-sided weakness, and is found to have a distal left M1 occlusion. He is treated with thrombectomy based on the time window, with TICI 2c reperfusion. He is admitted to the NCCU after thrombectomy. Maintenance fluids are ordered at 100mL/hr as he's NPO pending an SLP evaluation the next morning. Permissive hypertension is set, with goal BP < 180/105.
On day 3 of admission, you obtain the usual daily labs, and see that his Cr has risen quite a bit.
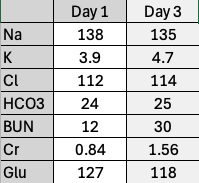
Yes. His serum creatinine has increased by ≥ 0.3mg/dL within the past two days.
What about the etiology? You might be tempted to say pre-renal, as it usually is, statistically. Let's say that you obtain urine studies and the FeNa indicates that this is a pre-renal state. Done! Give fluids, right?
Not necessarily. While a pre-renal state is often due to hypovolemia, there's another key possibility to consider. This patient has HFrEF with a low LVEF. We've been giving him maintenance fluids after he came in with an acute stroke. Let's go back to examine the patient. Here, let's say he has an elevated JVP. On point-of-care ultrasonography, he has diffuse B-lines, a dilated IVC, D > S wave on hepatic vein Doppler, and an increase in portal vein pulsatility. All of these signs point to venous congestion. Thus, the solution here would to be diurese him, not to give him more fluid.