A 59 year-old woman with NIDDM2 and CKD2 (baseline Cr 1.2) is admitted post-operatively after undergoing L3-S1 posterior instrumented fusion. Estimated blood loss was 100mL. She received one unit of packed red blood cells in the OR. Post-op labs are stable compared with prior. A Foley catheter was placed in the OR and remains in place.
On day 2 of admission, she becomes hypotensive down to a MAP of 35. You re-check a CBC, which shows a stable hemoglobin of 11.5, and give 1L of LR. Her BP momentarily responds, but then starts drifting down again. You utilize some non-invasive ways of assessing fluid responsiveness, and determine that additional fluid would not be helpful. So, you start norepinephrine gtt. You send off a repeat BMP and coags.
On day 3 of admission, you get the usual daily labs. You perform a focused cardiac exam, and find no signs or symptoms suggestive of hypo- or hypervolemia.
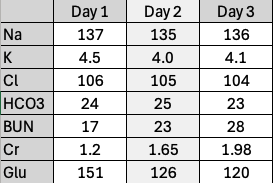
Yes. Her serum creatinine has increased by ≥ 0.3mg/dL within the past two days. She has an AKI-on-CKD.
What about the etiology? Even without sending urine studies, there are two possibilities to expect. First is the always-cited pre-renal cause of hypovolemia. Possible, but there didn't seem to be that much blood or volume loss around when this started. Second is the sometimes-forgotten cause of hypotension, which can really lead to an intrarenal AKI with ATN. Assuming she does truly appear euvolemic even on day 3, her Cr is still rising. This is likely still from this episode of hypotension +/- hypovolemia; it should begin to plateau soon.