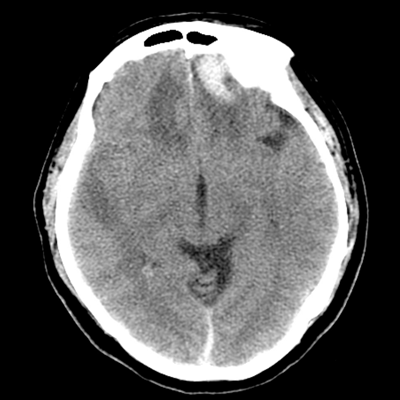
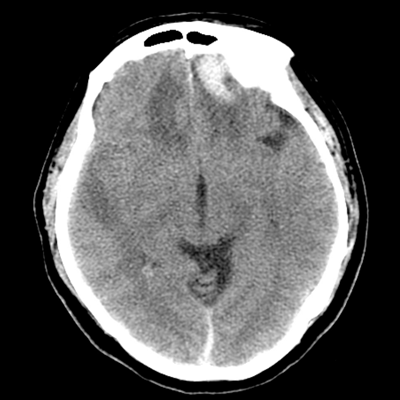
A 61 year-old man with HTN and NIDDM2 trips and falls at work, hitting the back of his head. He does not lose consciousness. His manager calls 911, and he is brought to the ED by EMS. There, he is agitated and combative. He is sedated with haloperidol, facilitating acquisition of cross-sectional imaging. A non-contrast head CT, shown here, and CTA head/neck are obtained. You note a large left > right frontal IPH with some hypoattenuation, and no IVH. He is admitted to the NCCU for further monitoring and management. On day 4 of admission, he sustains an acute neurologic decline, becoming markedly somnolent. You intubate him for airway protection. Which of the following tests should you order next to confirm your suspicion of the etiology of this decline?
While cEEG would be reasonable (note that the sensitivity might be poorer given the frontal lobe location of his abnormalities), there is another more pressing test to obtain first.
It's important to be cautious about getting MRIs for acutely neurologically ill patients who are at risk for herniation and intracranial hypertension. Progressive cerebral edema in the time window given in the vignette should be of concern, and so there's another test that can help provide an answer more quickly (even if not with as much resolution). If the CT scan done before this is reassuring and the clinical situation is appropriate, MRI could be obtained thereafter.
Yes! Bilateral frontal contusions/IPH with vasogenic edema are at high risk of developing progressive cerebral edema in the first few days. (Hematomas may also expand, so that'd be worth investigating.) Some even suggest routinely obtaining surveillance scans in this time window so as to identify whether this edema-- which can be clinically occult-- is developing. In this case, vessel imaging could also help identify vasospasm, which can also occur in TBI (though to a lesser extent than aSAH).
Viscoelastic assays such as TEG and ROTEM can be useful when trying to decide what products to transfuse. However, in this clinical vignette, a coagulopathy was not mentioned, and they would not be helpful in isolation anyway. Another test is of higher priority.
Post-traumatic vasospasm is possible, but TCD is not the best modality to identify this, at least not in the hyperacute setting. TCDs are more useful for identifying trends than absolute values.