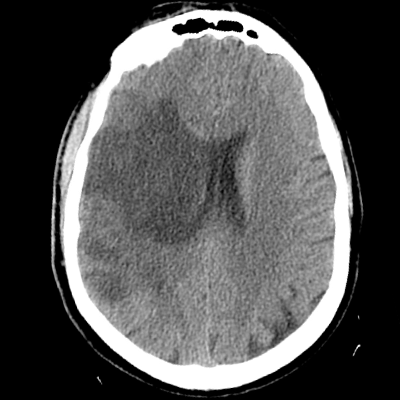
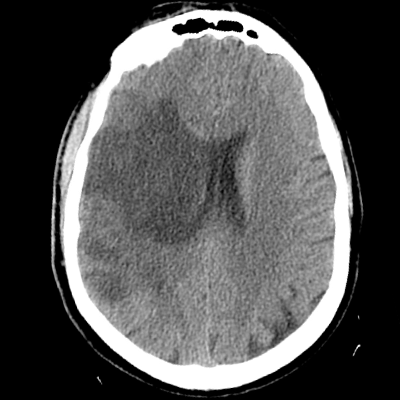
A 41 year-old man with regular marijuana use presents to the ED with an acute onset of dysarthria and left hemiparesis, approximately two hours from his last known normal. On exam, you note anosognosia, neglect of his left hemibody, and left hemiparesis. He is treated with tPA and undergoes successful thrombectomy of his right M1 occlusion. He's admitted to the NCCU. Post-procedurally, his exam demonstrates spontaneous alertness, persistent dysarthria, and improved left-sided strength. On post-stroke day 2, he becomes more somnolent, and his left side is now plegic. You obtain the following STAT non-contrast HCT. You get the patient intubated for airway protection. You administer 30mL of 23.4% NaCl. What is the next best step?
This would not be recommended as mannitol, with its reflection coefficient of 0.9, would eventually cross the blood-brain barrier and into the infarcted parenchyma. Free water would follow, causing rebound cerebral edema. Even if it weren't for this physical property, it's important to remember that this would only be a temporizing maneuver. There's a better alternative step that must be pursued next.
We've already given an aliquot of 23.4%. Hyperosmolar therapy in this setting is a temporizing maneuver that might help improve mass effect as this patient is beginning to herniate. However, it is not a definitive therapy, and there is a better alternative step that must be pursued next.
Yes! This patient is young (age < 60), has > 50% of his MCA territory infarcted, and is within 48 hours of his infarct. While you can still do some temporizing maneuvers such as hypertonic saline, you must act quickly as systematic reviews identify a clear mortality AND morbidity benefit to early DHC (done within 48 hours) for patients with malignant MCA strokes aged < 60. Hyperosmolar therapy does not replace the need for DHC, which is the definitive treatment in this case.
This would be incorrect, as the underlying problem-- worsening mass effect with herniation from the large MCA infarct-- would not be addressed with CSF diversion. While EVD placement might become necessary, it should only be considered as an adjunct to DHC, which would be the definitive therapy. Placement of a left-sided EVD in this patient without decompression would increase the pressure gradient right to left, raising the risk of exacerbating the leftward midline shift.
This would not be a helpful step, as it wouldn't change management (he already underwent thrombectomy and would not undergo a repeated attempt for a re-occlusion), and there is another more pressing treatment choice to make that would go after the primary problem he currently faces: herniation.