You are urgently called to evaluate the patient due to an acute neurologic decline on day 3 of admission.
You call the primary team back as you rush over to the patient's room. The patient had suddenly developed severe head and neck pain, after which her left pupil became dilated and she became less responsive. Your neurology colleague is on their way over as well. The patient was fine earlier this morning. She had been a little agitated overnight, but improved this morning. They've still been unable to get that brain MRI due to agitation, and getting cEEG electrodes for 24 hours also delayed that.
You arrive at the patient's room. You quickly examine her. Her left pupil is truly dilated and unreactive. Her right pupil is also dilated and unreactive, and also deviates to the right. She is unable to follow commands but is moving her extremities spontaneously. The right side of her body seems to be moving slightly less than her left. You escort the patient with RRT and your neurology colleague to radiology, where a non-contrast head CT and CTA head/neck are obtained.


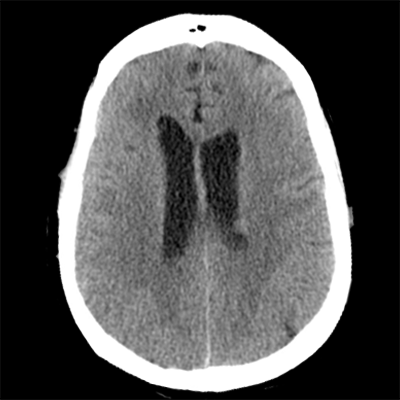

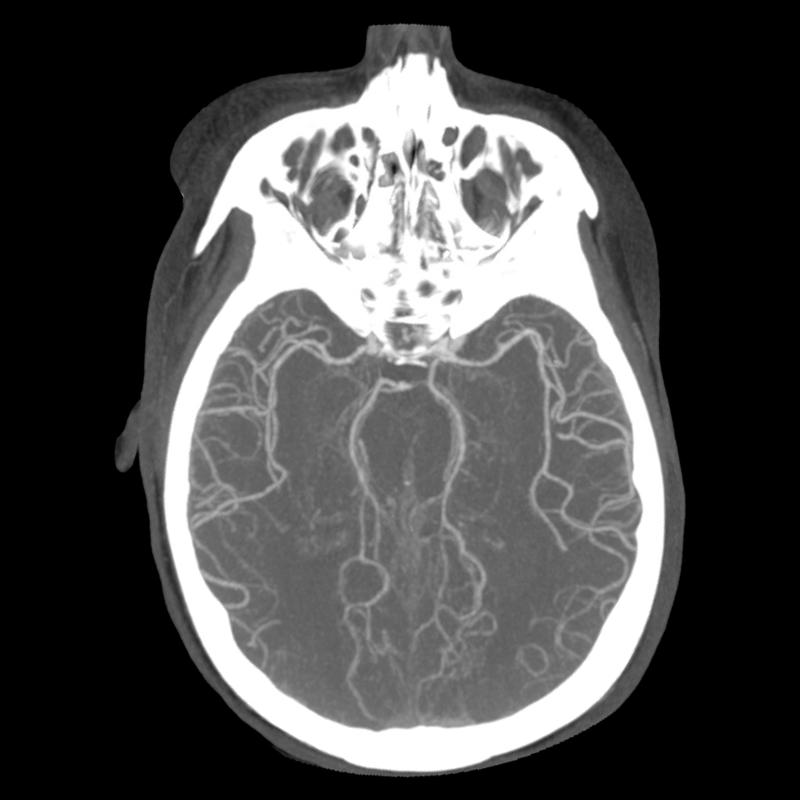
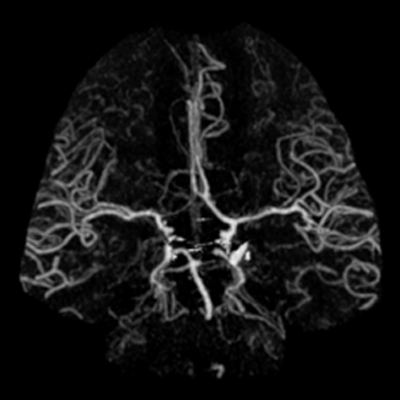
The non-contrast head CT looks generally similar to her prior scan. There's no new hemorrhage anywhere. There's no mass effect causing midbrain compression. The vessel imaging also looks unrevealing-- a slightly hypoplastic right A1 segment, but no clear LVO in either the anterior or posterior circulation. There's no vasoconstriction.
There was no new radiographic finding. So there's still no indication for acute neurosurgical intervention, right? However, her clinical decline is definitely new, so we haven't ruled out anything except any new radiographically-apparent structural etiologies. We need to ask ourselves if there's another etiology at play. We had thought she had just been having seizures, with which neurology agreed and was managing with ASMs. This precipitous decline warrants a reevaluation of what's been happening over the past week.
This is a woman with known metastatic melanoma that has progressed despite two different courses of immunotherapy. She had some brief episodes lasting < 1 minute of BUE shaking and impaired mentation. These episodes were never captured on EEG. EEG didn't show any epileptiform findings, but did have some abnormalities secondary to her known structural abnormalities of her prior right frontal tumor resection and leptomeningeal disease. It turns out she's had continued intermittent episodes of shaking despite levetiracetam monotherapy, and now she's had a precipitous decline in her mentation with her left pupil being blown. The acute decline could be sequentially related to the unknown, potentially unifying underlying etiology (i.e. melanoma metastasis that then bled, with the latter causing this sudden decline). Alternatively, this acute decline could be the culmination of whatever caused these prior unusual episodes, which themselves have not yet had a clear satisfying answer. These are the most parsimonious explanations. An unlikely alternative is that the acute decline is wholly unrelated to what's been happening.
When we think of etiologies of episodic neurologic dysfunction, vascular events (e.g. TIAs, stuttering infarcts), seizures, and migraines are the most commonly mentioned. We already have vessel imaging that's unrevealing, and the clinical presentation wouldn't fit that anyway. We've already talked at length about seizures. Her EEG showed the expected focal findings, but never anything epileptiform. Seizures haven't actually been fully ruled in. Of course, the lack of epileptiform findings doesn't rule it out either. But would it make sense for seizures to present with this obtundation and blown pupil? (It shouldn't.) This patient is now critically ill and migraines don't make any sense for this, so we won't even go there.
While the above three causes may be the most common causes of episodic neurologic dysfunction, there are a few others. There's cortical spreading depolarization, which you probably have mainly heard in the context of migraines, but also occur with other brain pathologies such as delayed cerebral ischemia associated with aneurysmal subarachnoid hemorrhages. (For subarachnoid hemorrhage, symptomatic vasospasm can also cause episodic focal dysfunction that resolves with treatment.) Another one that's often neglected, but underappreciated and very pertinent to patients like this, is plateau waves.
Plateau waves are "intermittent episodes of neurologic dysfunction that result from sudden rises in intracranial pressure" (Posner et al 2019). The name is derived from the ICP waveform that you'd get with invasive monitoring. Is this patient at high risk of intracranial hypertension? YES! She has known leptomeningeal carcinomatosis that impairs CSF resorption. Now, it makes more sense that these prior episodes of intermittent shaking were plateau wave manifestations, with her ICP being higher each time. But, things have cascaded to the point where the ICP elevation has reached a critical point and is now sustained.