The patient goes to the OR later in the night and undergoes a successful T4-T5 decompression and T1-T7 posterior instrumented fusion. He returns to the NCCU intubated thereafter.
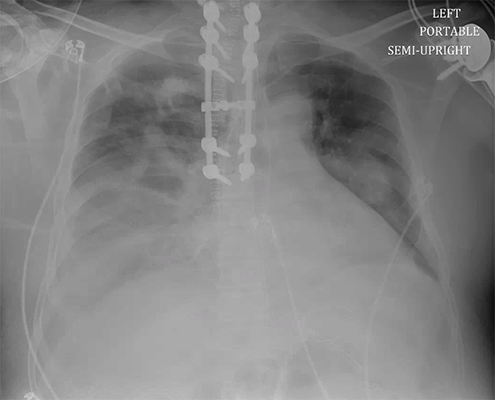
On day 3 of admission, he develops worsening hypoxemia, requiring an increase in PEEP to 10, as well as an increase in secretion burden. Based on the clinical history and the timing, with this increase in airway opacities, bacterial pneumonia (aspiration?) was of high suspicion. He was initiated on the appropriate antibiotics. At this point, with the increase in right pleural effusion on CXR, a diagnostic thoracentesis is performed-- bloody fluid is obtained. A pigtail chest tube is then placed for hemothorax, with 1L output.
He develops ARDS and requires prolonged ventilatory support. He undergoes a bedside percutaneous tracheostomy on day 14 of admission.
He is discharged to IPR on day 35 of admission.