The patient goes down to CT. The following images are obtained. The subdural fluid collection is stable, as is the ventricular caliber.
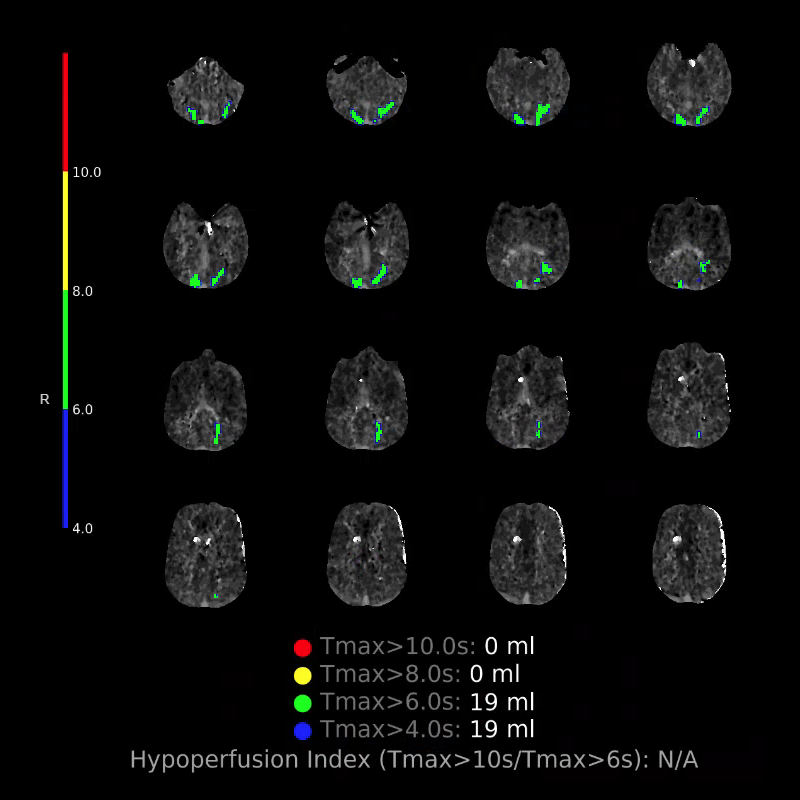
Starting with the non-contrast head CT, we can appreciate that there's actually not much residual subarachnoid blood at all; it's essentially all resorbed already (and cleared through the EVD). The ventricular caliber is stable. With the CTA head (for convenience's sake, the MIPs were shown), it's subtle, but we can see that the PCAs on each side are not as smooth and regular. The right MCA, starting at the bifurcation, also becomes narrower. This is [radiographic] vasospasm. Now, looking at the CT perfusion-- specifically, the Tmax (MTT) map that were selected-- there's clearly some abnormality within the bilateral cerebellar hemispheres and occipital lobes. Not a lot, but it's there. Delving further into this map, we can appreciate that the areas of abnormality are mainly green, signifying that these areas have Tmax > 6 seconds. This is the threshold that is specific, not sensitive, for vasospasm.
Putting this all together, we have thus identified radiographic vasospasm with the vessel imaging, with perfusion abnormalities that are concordant with it. Does the area of vasospasm and hypoperfusion correlate with the patient's clinical exam?
Yes! It does. The patient had a decline in level of consciousness with diffuse loss of motor function. This does correlate to the basilar territory. (Alternatively, bilateral MCA vasospasm could also be responsible, reminding us that a decline in consciousness could technically be focal/multifocal.) Thus, we can say that this patient does have clinical vasospasm. Whether this will develop into irreversible DCI remains to be seen; at least, the non-contrast head CT and the other portions of the CT perfusion (not shown) currently don't [yet] suggest infarction.